GLYXAMBI®
Consumer Medicine Information (CMI) summary
The full CMI on the next page has more details. If you are worried about taking this medicine, speak to your doctor or pharmacist.
1. Why am I taking Glyxambi?
Glyxambi contains the active ingredients empagliflozin and linagliptin. Glyxambi is
used to lower blood sugar levels in patients with type 2 diabetes mellitus and may
be used when diet plus exercise do not provide adequate blood sugar level controls
either alone or with certain other medicines for diabetes such as metformin.
For more information, see Section 1. Why am I taking Glyxambi? in the full CMI.
2. What should I know before I take Glyxambi?
Do not take Glyxambi if you have ever had an allergic reaction to the active ingredients
(empagliflozin and/or linagliptin) or any of the ingredients listed at the end of
the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines,
or are pregnant or plan to become pregnant or are breastfeeding.
For more information, see Section 2. What should I know before I take Glyxambi? in the full CMI.
3. What if I am taking other medicines?
Some medicines may interfere with Glyxambi and affect how it works.
A list of these medicines is in Section 3. What if I am taking other medicines? in the full CMI.
4. How do I take Glyxambi?
Your doctor will tell you how many tablets you need to take each day. The usual dose is one tablet once a day.
More instructions can be found in Section 4. How do I take Glyxambi? in the full CMI.
5. What should I know while taking Glyxambi?
|
Things you should do |
|
|---|---|
|
Things you should not do |
|
|
Driving or using machines |
|
|
Drinking alcohol |
|
|
Looking after your medicine |
|
For more information, see Section 5. What should I know while taking Glyxambi? in the full CMI.
6. Are there any side effects?
Common side effects include: constipation, cough, swelling of the nose or throat, mouth ulceration or itching. Serious potential side effects that may require medical attention include: low blood sugar (when used in combination with other anti-diabetic medicines); dehydration; burning sensation when passing urine; cloudy urine; straining or pain when passing urine; and pain in the pelvis or mid-back. Side effects that require urgent medical attention include swelling of the penis; bullous pemphigoid; pancreatitis; Fournier's gangrene; allergic reactions and diabetic ketoacidosis. For more information, including what to do if you have any side effects, see Section 6. Are there any side effects? in the full CMI.
GLYXAMBI®
Active ingredients: empagliflozin and linagliptin
Consumer Medicine Information (CMI)
This leaflet provides important information about taking Glyxambi. You should also speak to your doctor or pharmacist if you would like further information or if you have any concerns or questions about taking Glyxambi.
Where to find information in this leaflet:
1. Why am I taking Glyxambi?
Glyxambi contains the active ingredients empagliflozin (which belongs to a group of medicines called SGLT2 inhibitors) and linagliptin (belongs to a group of medicines called DPP-4 inhibitors). Both medicines work together to control blood sugar levels in patients with type 2 diabetes mellitus by increasing the amount of glucose expelled in urine, and producing more insulin to lower blood sugar levels.
It may be used when diet plus exercise does not provide adequate blood sugar level control either: alone or with certain other medicines for diabetes such as metformin.
Type 2 diabetes mellitus (or non-insulin-dependent diabetes mellitus or NIDDM) develops if the body does not make enough insulin or if the insulin that your body makes does not work as well as it should.
Lowering and controlling blood sugar levels may help prevent or delay complications of diabetes, such as heart disease, kidney disease, blindness and foot amputation.
Continue to follow the diet and/or exercises recommended for you while you are on treatment with Glyxambi.
2. What should I know before I take Glyxambi?
Warnings
Do not take Glyxambi if:
- you are allergic to empagliflozin or linagliptin, or any of the ingredients listed at the end of this leaflet.
Tell your doctor if you:
- take any medicines for any other condition
- have allergies to any other medicines, foods, preservatives, or dyes.
- have or have had any of the following medical conditions:
- type 1 diabetes, a condition where your body does not produce insulin.
- diabetic ketoacidosis, a condition in which substances called 'ketone bodies' accumulate in the blood and which can lead to diabetic pre-coma. Symptoms include: rapid weight loss, feeling sick or being sick, stomach pain, excessive thirst, fast and deep breathing, unusual sleepiness or tiredness, a sweet smell to your breath, a sweet or metallic taste in your mouth, or a different odour to your urine or sweat.
- kidney problems
- a disease of the pancreas
- illnesses that will make you dehydrated (e.g. diarrhoea or a severe infection)
- frequent genital or urinary tract infections (infections of the bladder, kidney, or tubes that carry urine)
- increased urine loss which may affect the fluid balance in your body
- heart problems, a history of low blood pressure or are 75 years of age or older, your risk of dehydration might be increased.
During treatment, you may be at risk of developing certain side effects. It is important you understand these risks and how to monitor for them. See additional information under Section 6. Are there any side effects?
Pregnancy and breastfeeding
Do not take this medicine if you are pregnant.
It may affect your developing baby if you take it during pregnancy.
Do not breastfeed if you are taking this medicine.
It is not known whether the active ingredients in Glyxambi pass into human breast milk and there is a possibility that your baby may be affected.
Do not start taking Glyxambi if you are over 75 years of age.
Do not give Glyxambi to a child under the age of 18 years.
Safety and effectiveness in children younger than 18 years have not been established.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any medicines, vitamins or supplements that you buy without a prescription from your pharmacy, supermarket or health food shop.
Some medicines may interfere with Glyxambi and affect how it works-
- medicines used to treat high blood pressure known as water pills (diuretics)
- rifampicin (an antibiotic medicine used to treat certain infections such as tuberculosis)
- carbamazepine, phenobarbital (phenobarbitone) or phenytoin (medicines used to control fits (seizures) or chronic pain)
- a medicine used to treat and prevent mood disorders (lithium)
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins or supplements you are taking and if these affect Glyxambi.
4. How do I take Glyxambi?
Follow all directions given to you by your doctor or pharmacist carefully.
They may differ from the information contained in this leaflet
How much to take
The recommended dose is Glyxambi 10 mg/5 mg tablet once a day.
Your doctor may increase your dose to Glyxambi 25 mg/5 mg tablet once a day.
Your doctor will prescribe Glyxambi alone or in combination with another anti-diabetic medicine if that medicine alone is not sufficient to control your blood sugar level.
Continue taking your medicine for as long as your doctor tells you.
This medicine helps to control your condition, but does not cure it. It is important to keep taking your medicine even if you feel well.
When to take Glyxambi
Take your medicine at about the same time each day.
Taking it at the same time each day will have the best effect. It will also help you remember when to take it.
It does not matter if you take this medicine before or after food.
How to take Glyxambi
Swallow the tablet whole with a full glass of water.
If you forget to take Glyxambi
If you miss your dose at the usual time, and it is almost time for your next dose (less than 12 hours), skip the dose you missed and take your next dose when you are meant to.
Otherwise, take it as soon as you remember, and then go back to taking your medicine as you would normally.
Do not take a double dose to make up for the dose you missed. This may increase the chance of you getting an unwanted side effect.
If you are not sure what to do, ask your doctor or pharmacist.
If you take too much Glyxambi
If you think that you have taken too much Glyxambi, you may need urgent medical attention.
You should immediately:
- phone the Poisons Information Centre
(by calling 13 11 26), or - contact your doctor, or
- go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
5. What should I know while taking Glyxambi?
Things you should do
- Remind any doctor, dentist or pharmacist you visit that you are taking Glyxambi, especially if you are about to start any new medicine or if you are going to have surgery.
- Tell your doctor immediately if you become pregnant while taking Glyxambi.
- Tell your doctor that you are taking this medicine, if you are about to have any blood or urine tests. It may interfere with the results of some tests.
- Keep all your doctor's appointments so that your progress can be checked. Your doctor may do some tests from time to time to make sure the medicine is working and to prevent unwanted side effects.
- Follow your doctor's and/or dietician's advice on diet, drinking alcohol and exercise. Diet and exercise can help your body use its blood sugar better. It is important to stay on the diet and exercise program recommended by your doctor while taking Glyxambi.
- Check your blood sugar levels regularly. This is the best way to tell if your diabetes is being controlled properly. Your doctor or diabetes educator will show you how and when to do this.
- Check your feet regularly and see your doctor if you notice any problems. Follow any other advice regarding foot care given by your doctor.
- Talk to your doctor if you are about to have surgery. The doctor will provide instructions on when to stop and restart Glyxambi.
Things you should not do
- Do not take Glyxambi to treat any other complaints unless your doctor tells you to.
- Do not give your medicine to anyone else, even if they have the same condition as you.
- Do not stop taking your medicine or change the dosage without checking with your doctor.
Things to be careful of
Be careful when doing any of the following things, which may increase the risk of your blood sugar becoming too low:
- Drinking alcohol
- Not eating enough
- Doing unexpected or vigorous exercise
Driving or using machines
Be careful before you drive or use any machines or tools until you know how Glyxambi affects you.
When Glyxambi is taken with other anti-diabetic medicines, such as sulfonylurea or insulin, it can increase the risk of your blood sugar levels becoming too low. Low blood sugar can cause dizziness, lightheadedness, tiredness, drowsiness, and slow your reaction time, which can affect your ability to drive or operate machinery.
If you have any of these symptoms, do not drive, operate machinery or do anything else that could be dangerous.
Drinking alcohol
Tell your doctor if you drink alcohol.
Alcohol may increase the risk of your blood sugar becoming too low.
Looking after your medicine
- Keep your medicine in a cool, dry place where the temperature stays below 30°C. Protect from heat and dampness.
- Keep the tablets in the blister strip until it is time to take them.
Follow the instructions in the carton on how to take care of your medicine properly.
Do not store it:
- in the bathroom or near a sink, or
- in the car or on window sills.
Keep it where young children cannot reach it.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you have any further questions about side effects.
Do not be alarmed by the following list of side effects. You may not experience any of them.
Less serious side effects
|
Less serious side effects |
What to do |
|---|---|
|
Stomach related disorders:
Nasopharyngeal disorders:
Urinary disorders:
General body disorders:
|
Speak to your doctor if you have any of these less serious side effects and they worry you. |
Serious side effects
|
Serious side effects |
What to do |
|---|---|
|
Symptoms of low blood sugar:
Low blood sugar may occur in patients who already take another medication to treat diabetes, such as a sulfonylurea or insulin. The dose of your sulfonylurea or insulin medicine may need to be reduced while taking Glyxambi. Symptoms of dehydration:
Symptoms of urinary tract infection:
|
Speak to your doctor as soon as possible if you have any of these serious side effects. |
Very serious side effects:
|
Very Serious side effects |
What to do |
|---|---|
|
Symptoms of Bullous pemphigoid:
Symptoms of Fournier’s gangrene:
Symptoms of an allergic reactions:
Symptoms of inflamed pancreas (pancreatitis):
Effects on genital organs:
Symptoms of diabetic ketoacidosis:
In rare cases, empagliflozin, one of the active substances in Glyxambi can cause a serious side effect called diabetic ketoacidosis. The symptoms of diabetic ketoacidosis may continue in some patients after they stop taking Glyxambi. |
Call your doctor straight away or go straight to the Emergency Department at your nearest hospital if you notice any of these very serious side effects. |
Tell your doctor or pharmacist if you notice anything else that may be making you feel unwell.
Other side effects not listed here may occur in some people.
Some of these side effects can only be found when your doctor does tests from time to time to check your progress.
Reporting side effects
After you have received medical advice for any side effects you experience, you can report side effects to the Therapeutic Goods Administration online at www.tga.gov.au/reporting-problems. By reporting side effects, you can help provide more information on the safety of this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What Glyxambi contains
|
Active ingredient (main ingredient) |
Each Glyxambi 10 mg/5 mg tablet contains 10 mg empagliflozin and 5 mg linagliptin Each Glyxambi 25 mg/5 mg tablet contains 25 mg empagliflozin and 5 mg linagliptin |
|---|---|
|
Other ingredients (inactive ingredients) |
|
|
Potential allergens |
None |
Do not take this medicine if you are allergic to any of these ingredients.
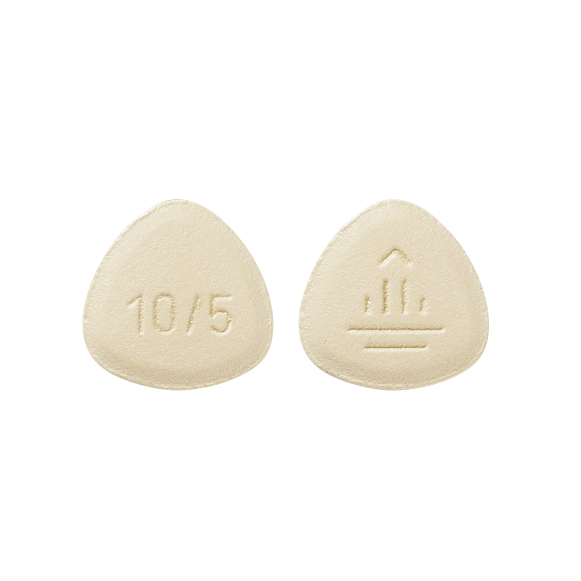
What Glyxambi looks like
- Glyxambi 10 mg/5 mg tablets are pale yellow, arc triangular, flat-faced, bevel-edged, film-coated tablets. One side is debossed with the Boehringer Ingelheim company symbol, the other side is debossed with "10/5". (AUST R 263556)
- Glyxambi 25 mg/5 mg tablets are pale pink, arc triangular, flat-faced, bevel-edged, film-coated tablets. One side is debossed with the Boehringer Ingelheim company symbol, the other side is debossed with "25/5. (AUST R 263557).
Glyxambi is available in blister packs containing 10 (sample) and 30 tablets.
Who distributes Glyxambi
Glyxambi is supplied in Australia by:
Boehringer Ingelheim Pty Limited
ABN 52 000 452 308
Sydney NSW
www.boehringer-ingelheim.com.au
This leaflet was prepared in April 2025.
® Glyxambi is a registered trademark of Boehringer Ingelheim.
© Boehringer Ingelheim Pty Limited 2025.
 Download PDF >
Download PDF >